Astronauts can get a head-rush too!
The outcomes of the SANS-CM study on how we can tackle Orthostatic Intolerance in Space and on Earth.
The problem
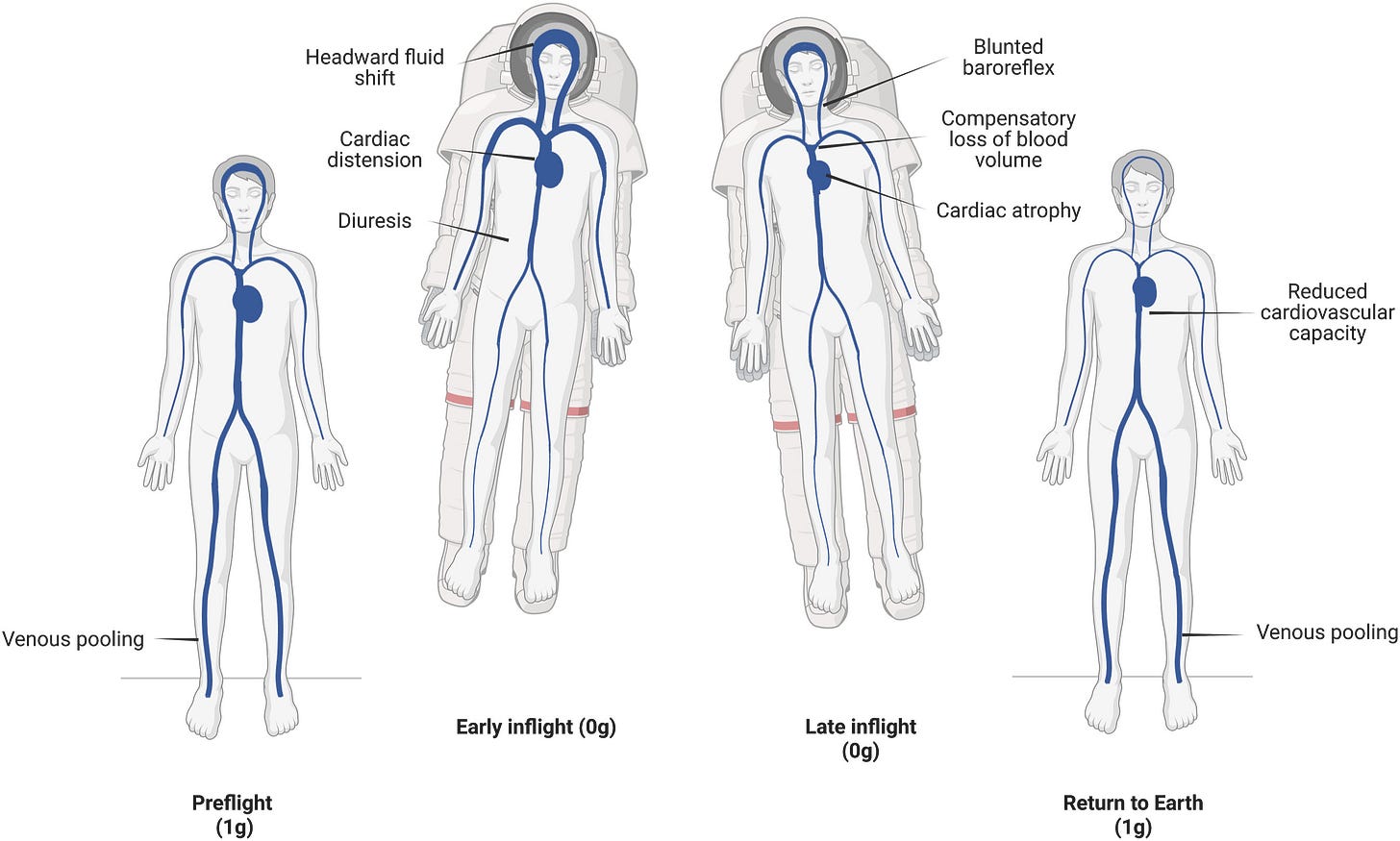
Orthostatic Intolerance in astronauts can be impactful on mission success and even be life-threatening, specially when dealing with emergency situations or when landing on celestial bodies. 🛸
Some causes that are currently on the table:
Weightlessness-induced cardiovascular deconditioning.
Reduced blood volume.
Altered neurohumoral cardiovascular control.
Countermeasures currently in place:
Lower body negative pressure (LBNP), where a device pulls the blood back into the legs, simulating the physiological state of venous pooling in the lower extremities, 0.5 to 1 hours every other day.
Physical exercise, in some high-end machines, 2 to 3 hours per day.
However, these are not enough. Astronauts still need to be carried out of their ships after landing and experience orthostatic intolerance long after they’ve landed. How can we solve this?
The (proposed) solutions
Hönemann and team sought to see the impact of these two solutions:
Increasing the daily exposure of LBNP (to 6 hours, daily)
A cycling + daily thigh cuffs protocol, combining exercise and forced venous pooling (by diminished venous drainage)
Methods
The team took 47 healthy volunteers and tested-out their two solutions. But how?
Exposure
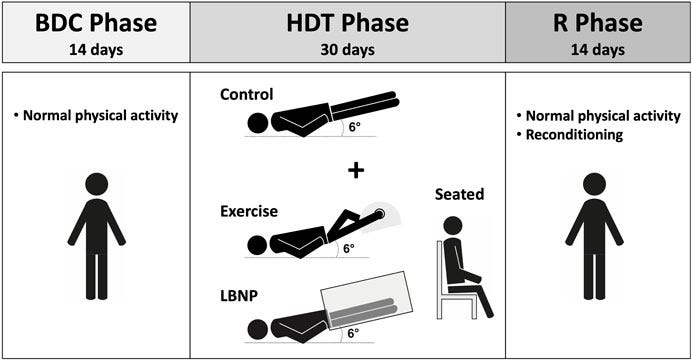
To simulate microgravity on Earth, we can place subjects in Head Down Tilt at a 6-degree angle. Subjects are laid in bed at an angle that changes the vector just enough that gravity pulls everything to the the head with the right force, simulating the headward shift of organs and fluids that is observed in microgravity.
For how long, you ask? 30 days!
Comparison
The team created four groups:
Group in Head Down Tilt with solution number 1 (LBNP)
Group in Head Down Tilt with solution number 2 (cycling + cuffs)
Negative Control Group in Head Down Tilt with nothing else (expect to see orthostatic intolerance here)
Positive Control Group in Head Down Tilt but got to sit up for 6 hours per day (expect to not see that much orthostatic intolerance here)
Outcomes
The data that was collected in each of the four groups tried to answer the question and also provide some insight on what was happening:
Orthostatic Tolerance testing, quantifiable as the time between the beginning of the test and the onset to pre-syncope - i.e. a very aggressive form of head-rush.
Circulating blood insights, such as plasma volume, blood volume and total mass of red-blood cells.
Results
Solution 1 (LBNP) alleviated orthostatic intolerance just as much as sitting upright. Both these groups had higher plasma volume losses that the other two.
Solution 2 (cycling + cuffs) kept plasma volume the same but didn’t help much with orthostatic tolerance.
No group was left without orthostatic intolerance, not even the group that was allowed to sit up!
Take home messages
Lower Body Negative Pressure appears to be our best shot so far to mitigate orthostatic intolerance in Space.
Maybe even a solution for helping bed-ridden patients on Earth.
There are no perfect solutions yet!
Even sitting for 6 hours a day is not enough, so move!
Plasma volume may not have that much to do with orthostatic tolerance as we once thought, and we still clearly have a long road ahead.
References
Hönemann JN, Hoffmann F, de Boni L, et al. Impact of Daily Lower-Body Negative Pressure or Cycling Followed by Venous Constrictive Thigh Cuffs on Bedrest-Induced Orthostatic Intolerance. J Am Heart Assoc. 2024;13(21):e034800. doi:10.1161/JAHA.124.034800
Thoolen SJJ, Kuypers MI. External Hemorrhage Control Techniques for Human Space Exploration: Lessons from the Battlefield. Wilderness Environ Med. 2023;34(2):231-242. doi:10.1016/j.wem.2023.01.006
Clément G, Moudy SC, Macaulay TR, Mulder E, Wood SJ. Effects of intermittent seating upright, lower body negative pressure, and exercise on functional tasks performance after head-down tilt bed rest. Front Physiol. 2024;15:1442239. Published 2024 Sep 6. doi:10.3389/fphys.2024.1442239